Welcome to our Paediatric First Aid page, your guide to understanding and addressing some (but definitely not all!) common childhood injuries and illnesses from A to Z. Here, you'll find detailed information and practical tips to help you manage various health concerns children may face. However, please note that this information is not a substitute for professional medical advice. If you have any concerns about your child's health, we strongly recommend seeking immediate medical attention. For those looking to deepen their knowledge and skills in paediatric first aid, we offer a face-to-face course that provides hands-on training and expert guidance.
Anaphylaxis
Anaphylaxis is a life-threatening allergic reaction that happens very quickly. It can be caused by food, medicine or insect stings. The reaction usually starts within minutes of coming into contact with the allergen. You should call 999 immediately if you think yourself or someone else if having an anaphylactic reaction. Symptoms can include:
Hoarse Voice / Wheeze / Stridor
Swelling of the throat and tongue, which causes difficulty breathing / fast breathing / difficulty swallowing / tightness in the throat.
Tiredness / confusion / feeling faint.
Skin that feels cold to the touch / blue, grey or pale skin, lips or tongue
A rash that's swollen, raised or itchy.
1) Use an EpiPen if you have one (Instructions are written on the device
2) Call 999
3) Lie the person on their back and raise their legs, if they are struggling to breath, sit them up slightly.
Burns
A burn is created by dry heat, such as fire or a hot surface. A scald is created by wet heat, such as hot water or steam. Both are very painful, however the amount of pain does bot indicate how serious the burn is- Some of the most serious burns aren't always that painful. The skin can appear red, blistered, white or swollen depending on the type of burn. There are 4 main types of burn: Superficial epidermal burn, Superficial Dermal Burn, Partial Thickness burn, Full Thickness burn.
1) Move the child away from the heat source and to a place of safety.
2) if possible, remove any clothing from the area including jewellery. If the clothing is stuck to the child, leave it in place.
3) Run cool / tepid water over the area for no less than 20 minutes. This could be quite distressing for the child- Giving pain relief such as Calpol is a good idea! Whilst doing water therapy, ensure the child is warm, use a blanket around the child avoiding the area of burnt skin.
4) Cover the burn- Cling film is ideal! Covering the burn will protect against germs and also act as a good pain relief. Don't use any sticky dressings or creams such as sudocream / tooth paste / butter.
5) If possible, raise the affected area to help reduced swelling.
6) Attend a walk in centre / A&E for further advise and ongoing treatment. This is especially important if the burn is on the face, neck, hands, feet, buttocks, genitals or over any joints.

Croup
Croup is often caused by a viral infection affecting the upper airway. It is most common in children between 6 months and 5 years. It has different levels of severity, from mild to life threatening. Croup symptoms can last for a few days and are usually worse at night time.
Symptoms include:
Temperature, runny nose, hoarse voice, a barking cough. In moderate - severe cases, symptoms can include a tracheal tug (Sucking in at the neck) and a stridor (High pitched breathing sound caused by an obstruction to the upper airway). Croup symptoms can be very similar to symptoms of foreign body, airway trauma or smoke inhalation, so if in doubt- get checked out!
Treatment pre hospital can include:
1) Calpol and ibuprofen for temperature relief and assisting with reducing the inflammation in the airway.
2) The care giver staying calm to promote the child staying calm. Often distress can exacerbate croup symptoms.
3) Standing outside in cool air for 15 minutes has been found to improve symptoms. Ensure your child is kept warm if you choose to stand outside.
Usually croup will improve on its own within 48 hours, however in some cases, a trip to A&E is required for a steroid called Dexamethasone. In severe cases nebulised adrenaline may also be required.
Dog Bites
Most Dog bites (Or other animal / human bites) are not serious, however you may need to get medical treatment if the bite is severe, on a key area such as hands, feet, face or there are signs of infection.
At the time of the incident:
1) Clean the area with soap and water
2)Remove any foreign body from the wound such as teeth / dirt under running water- Give Paracetamol / ibuprofen to ease the pain.
3) Let the wound bleed slightly, or squeeze gently to make it bleed- This can help reduce infection risk
4)Dry the wound and apply a clean dressing
5) Check your vaccination status- The hospital may want to give treatment for tetanus and rabies. They may also give antibiotics.
You should also strongly consider reporting the dog bite to 101.

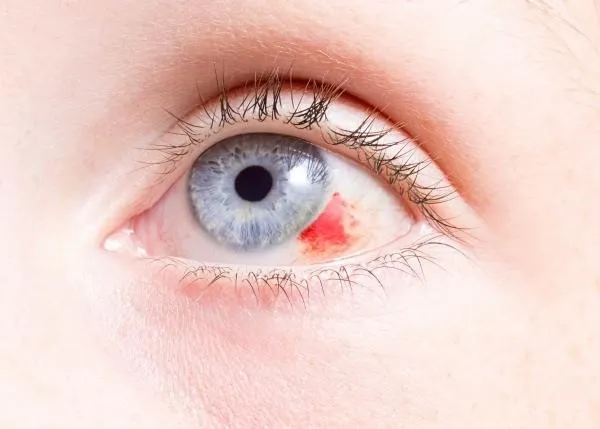
Eye Injuries
Minor eye injuries, such as body wash or dust in the eye, often get better on their own. However the eye can feel quite irritated and sore. You should go to your local A&E if the child has a chemical (Such as diffuser oil / cleaning product ) in the eye or something pierces it (Such as a pen nib / nurf gun bullet!)
1) Wash the eye with running water for as long as can be tolerated (Up to 20 minutes)
2) Give paracetamol / ibuprofen to ease the pain
3) Look at the advise on the packet for further management
If the Injury has made the eye bleed / visual disturbance / the child is being sick / The child cannot open their eye / The injury was high speed then go to A&E.
Febrile Convulsion
A Febrile Convulsion (Seizure) can happen when a child's temperature rises at a fast speed. It can be scary to watch!
The child may become stiff, twitch, shake. They may be unconscious or not respond when you talk to them. They may also wet themself or vomit.
The fit should only last a few minutes- Commence a timer at the start of the fit. Protect their head and remove any dangerous objects.
If the fit lasts more than 5 minutes, call 999. Regardless- Get the child checked over- It might be that the child had an underlying infection such as tonsilitis that needs treatment.

Head Injury
Head injuries in children are very common! They love exploring and testing their limits, which can sometimes result in injury. Depending on the symptoms and mechanism of the head injury will depend on you going to A&E. In minor head injuries:
1) apply a cold compress / frozen peas in a towel
2) Rest- you do not need to keep the child awake.
3) Take paracetamol to ease the discomfort
4) Ensure an adult stays with the child for the next 24 hours.
You would need to take the child to A&E if:
They lost consciousness (Call 999 if still unconscious!)
They have vomited after the head injury.
They had a seizure following the head injury (Call 999 if still fitting!)
The child becomes more irritable / change in behaviour or memory loss.
The child has had previous brain surgery or has a known blood condition such as haemophilia.
There is a wound to the head that needs to be closed.

Irritable Hip
Irritable hip is the most common cause of hip pain and/or limping in children. It is also known as transient synovitis. It usually gets better by itself within 1-2 weeks. It is most often seen in children aged 3-10 years. The pain and limp are due to inflammation of the lining of the joint and increased fluid inside the joint. The child may also have a mildly raised temperature and some children may have recently experienced a viral illness such as a cold, a sore throat or diarrhoea and vomiting.
1) Give pain relief such as ibuprofen or paracetamol.
2) Let the child rest until the symptoms have resolved. If the symptoms last longer than 2 weeks then arrange a GP appointment for further investigations.
3) Attend A&E if the child gets sudden pain in their hip, thigh or knee or the child is limping or cannot put any weight on 1 leg.

Kawasaki Disease
Kawasaki disease mainly affects children under the age of 5. It's also known as mucocutaneous lymph node syndrome. The condition causes the blood vessels to become inflamed and swollen. Generally, A child with Kawasaki disease has a high temperature that lasts for 5 days or longer and other symptoms such as: a rash, swollen glands in the neck, a swollen, bumpy, red tongue, swollen and red hands and feet. Kawasaki disease can't be prevented, but the children can make a full recovery if the condition is treated promptly! It's important to seek medical attention so that the intravenous treatment can get started in hospital. Without treatment, around 1 in 4 children with Kawasaki disease get heart complications.

Lyme Disease / Tick Bite
Lyme disease is a bacterial infection that can be spread to humans by infected ticks. Ticks that may cause Lyme disease are found all over the UK, but high risk places include grassy and wooded areas in southern and northern England and the Scottish Highlands.
A circular or oval shape rash can appear around a tick bite around 1-4 weeks after the initial bite, and can last for several weeks. Some people also get other symptoms such as: temperature, feeling shivery, headache, muscle / joint pain, tiredness / loss of energy. To remove a tick safely:
Use tweezers or a tick removal tool
Grasp the tick as close to the skin as possible.
Slowly pull upwards, try not to crush the tick!
Clean the bite with soap and water.

Measles
Measles is an infection that spreads very easily and can cause serious problems in some children. Having the routine MMR vaccine is the best way to prevent it. Measles usually starts with cold-like symptoms, followed by a rash a few days later. The rash is not usually itchy. Small spots can also appear in the child’s mouth too. Alongside the rash, children can also get other symptoms such as temperature, runny nose, sneezing, coughing, sore eyes. Its important to get medical attention if you think your child may have measles, especially if they are under 1, or have a weakened immune system.

Nose Bleeds
Nosebleeds are not usually serious. In children, they are pretty common, and most can be easily treated at home. Sometimes, you may need to see a GP, especially if your child is under 2, or has regular nose bleeds, or if the child has symptoms of anaemia or takes medication to prevent blood clots.
To help stop the nose bleed, encourage the child to:
Sit down and lean forward, with their head tilted forward.
Pinch their nose just above the nostrils for 10 to 15 minutes
Breathe through their mouth
Holding an icepack on top of the nose may also slow the bleeding down.
You should take your child to A&E if the bleeding has lasted longer than 10 - 15 minutes, They are swallowing blood which makes them vomit, they have had a head injury, they are feeling dizzy / weak.

Open wounds
Most wounds be treated at home and will start to heal in a few days, however some wounds may need to be treated by a healthcare professional if there's a risk of infection, there’s a foreign body in it (Such as glass) or the wound is more serious.
If there's nothing in the wound, put pressure on it using something clean such as a tea towel for 10 minutes. If the wound is on the child’s hand or arm, raise it above their head. If the wound is on their lower limb, lie down and raise it. This will help reduce the blood flow.
You would need to take the child to the local A&E if a wound has soil in it- the child may need a tetanus injection. You should also seek medical advice if the child has started to develop a temperature following a wound, or the wound smells or looks infected. Some wounds may need closing with steri-strips, medical glue or sutures.

Paronychia
A Paronychia is an infection that develops from barrier disruption or trauma to the skin surrounding the nail. The allows infection to enter. Paronychias can be quite painfull for children. The finger becomes, red, swollen and tender, and you can often see a build up off puss surrounding the nail.
They are most commonly caused by false nails, having hands in water a lot, finger sucking and nail biting. Most cases of acute paronychia resolve in 2–4 days with treatment. Treatment can involve draining the infection by creating a small opening, and giving the child antibiotics. Untreated infections may lead to the child loosing their nail.

Splinter
Splinters are very common in our little explorers- but luckily they can be easily removed. However, if the splinter is deep in the skin it can be difficult to remove and may need to be removed by a healthcare professional.
At home, try to grasp the splinter with tweezers as close to the skin as possible - and draw it out in a straight line.
Squeeze the wound carefully to encourage slight bleeding as this will help to remove any dirt.
Clean and dry the wound.
If the splinter site appears red, swollen, increasing pain or leaking pus, it may be infected and you should book your child a GP appointment.

X-Rays
An X-ray is a quick and painless procedure commonly used to produce images of the inside of the body. X rays are used a lot in the A&E department to diagnose fractures. X-rays are usually carried out in hospital by specialists called radiographers, although they can also be done by other healthcare professionals, such as dentists. They're mainly used to look at the bones and joints, although they're sometimes used to detect problems affecting soft tissue, such as internal organs.
If your child is having an x ray, you will most likely be allowed to go in the room with the child. You may have to wear a led jacket to protect yourself from the radiation or stand behind a screen.



